As treatment sequencing becomes more complex, and drug options more varied, it becomes even more important to help clinicians factor in patient perspectives when making treatment decisions.
In this article, Client Growth Director James Langridge defines what empathy in Healthcare is, why it’s so important, how we can start to create more of it (for better patient outcomes) and some recent examples that harness tech to achieve this.
What do we mean by empathy in Healthcare?
How many of you reading this article have engaged with a clinician and felt like you couldn’t be fully honest with them, or withheld an important question or piece of information because you felt intimidated, rushed or judged? How many of you left feeling dissatisfied with the outcome, like your needs were never fully heard?
In the context of Healthcare, empathy can be understood as a deep connection with a patient’s experiences and motivations along their health journey, so that at any given point in that journey, you better understand their needs, drivers and pain points.
Why does empathy matter?
A McKinsey Report stated that many patients feel that existing health systems don’t support their needs, and one in five patients feel misunderstood by their healthcare team. We see a similar pattern across research for many of our client’s brands – where there is a clear divergence between patient and clinician treatment goals. This is important because the ultimate goal in healthcare is patient happiness, which necessitates not only that their clinical needs are met, but also that their psychosocial needs are met. Frequently, evidence suggests that, whilst clinicians like to focus on clinical markers of success, they often neglect psychosocial markers of success.
One good example of this is the treatment of early-stage schizophrenia, as historically clinicians have focussed mainly on controlling symptoms of the disease (hallucinations, delusions, hyperactivity etc.) with less consideration of the impact of anti-psychotic side effects on the patient’s overall wellbeing. A consequence of this is that patients often gained weight and felt heavily sedated on treatment, which meant they were less able to socialise, maintain relationships and hold down a job. This resulted in lower quality of life and higher rates of drug non-adherence/ subsequent relapse - which actually made the schizophrenia worse over the long-term.
So, if we are too narrow in our focus just on clinical markers for success (and forget we are ultimately treating people, not p-values), then we risk simply exchanging one problem for another. This is why we need empathy in Healthcare. A better solution demands a better understanding of the problem – which includes both psychosocial needs as well as clinical needs.
How can we bring more empathy into healthcare?
Go to the jungle to understand how the lion hunts
There’s a popular quote in market research, “If you want to understand how a lion hunts, don't go to the zoo. Go to the jungle.” What this means is that, to truly empathise and connect with a patient’s experiences and motivations, you need to get out there and immerse yourself in their lived health journey. Talk to patients in their environment, partner with Patient Advisory Groups to get insights into their lived experience, bring the patient into the articulation of the problem AND the design of the solution. This is empathy in action – and this close collaboration will highlight the critical moments along the patient journey where their needs, drivers and pain points are not currently met.
Harness tech innovation to address the empathy gap
A common reason for clinician’s focussing mainly on clinical markers of success is limited time and head-space to do anything more. It takes a lot of time and effort to uncover a patient’s broader psychosocial needs, and a patient may not feel comfortable or unwilling to voice their needs. In this context, trained AI can help bridge this gap, playing the role of a highly-skilled detective that can quickly triage patients to identify and stratify their needs and map these to the right level of care.
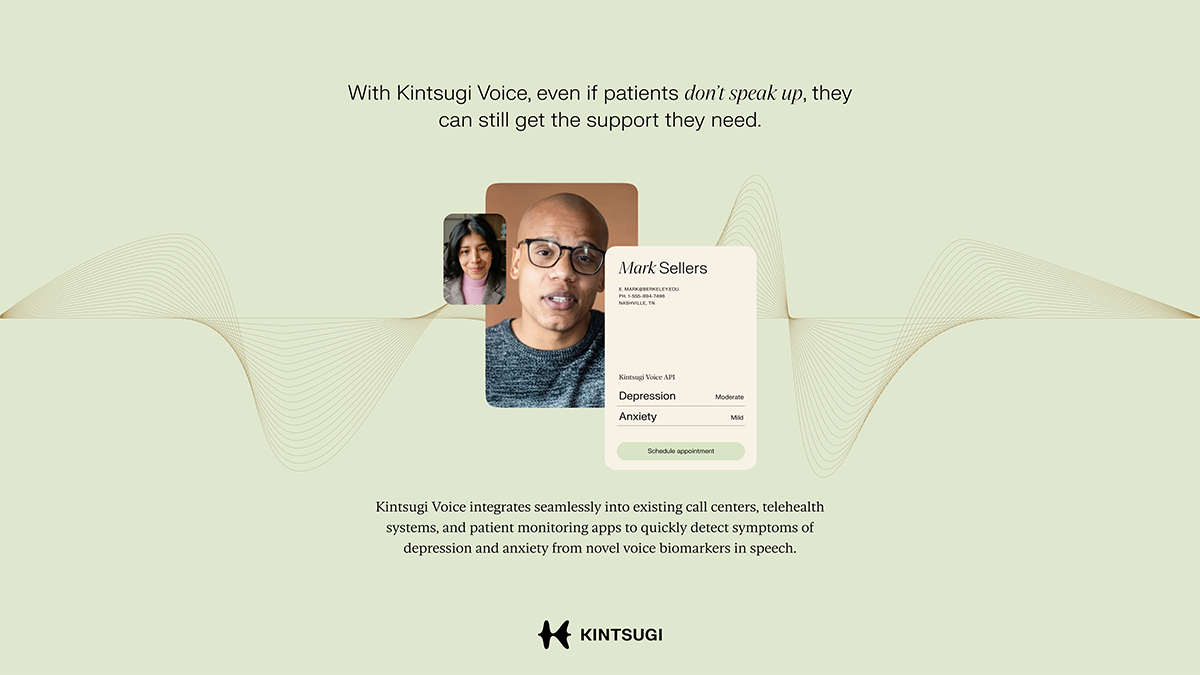
Not only can this alleviate responsibility on the time-poor clinician, but AI can detect signs and symptoms to identify patient needs with much greater sophistication and accuracy than humans. In one example below, voice bio-marker software was used to listen to patient-clinician conversations and detect signs of depression based on speech patterns. Furthermore, in this example, 80% of 800 patients were receptive to being assessed for mental health in this way, suggesting that patients welcome these moments for human connection and greater empathy that are created by AI.
The benefits of AI also stretch beyond improved assessment of mental health. For example, Orchard recently designed an AI patient support tool for patients with dementia, that was trained on resources from credible sources to deliver comprehensive patient support and information in a caring empathic voice, using the language of experienced care givers.
In summary, practicing Healthcare without empathy is like trying to play Chess when you can only see half of the board. What you might think is a good move for the patient may actually put them in a dangerous position. As trusted partners to clinicians, Pharma can help shine a light on the whole board, bringing empathy to the fore and ensuring that the next move is the right one.
Examples of empathy in action:
Kintsugi Voice Biomarker Technology
- Voice biomarker software that detects signs of clinical depression and anxiety based on listening to short recordings of patient/clinician conversations
- Integrated into clinical care management call centres, telehealth and remote patient management
Empatica medical-grade wearables
- Software and algorithms for the collection and interpretation of physiological data
- For people with autism, a big challenge is that others don’t understand their emotions (because they have a different ways of expressing them). Empatica measures autoimmune changes that correlate with specific emotions in a wearable, and the person can control who they then share this data with

Get in touch
Want to bring more patient-centricity into your brand and clinician engagements? Get in touch to see what we can create together. Reach out to james.langridge@orchard.com.au.

